Infectious microorganisms can survive on surfaces for weeks, months and even years if not removed. In the healthcare industry, for example, studies show that on average 50 per cent of surfaces remain contaminated, even as environmental services staff complete standard traditional cleaning.
New automated disinfection technologies are being implemented across the globe in an attempt to reduce or eliminate the environment as a potential path for these microorganisms to reach healthcare patients.
Among the most widely adopted include automated UV (ultraviolet) disinfection systems, which use UV-C energy to inactivate microorganisms at the genetic level by disrupting cellular DNA. These technologies should not replace traditional manual cleaning, but serve as a complementary tool. When used in addition to standard manual cleaning they have demonstrated a greater than a 99 per cent reduction in contamination of high touch surfaces.
Unfortunately, despite staggering statistics, the Canadian healthcare system has been slow to adopt these new technologies that have proven to reduce both environmental contamination and hospital acquired infection rates.
Hospital acquired infections are the third leading cause of death in Canada behind cardiovascular illness and cancer. According to a 2013 report by Canada’s chief public health officer, more than 200,000 Canadian patients will contract a healthcare acquired infection and more than 8,000 of them will die as a result each year.
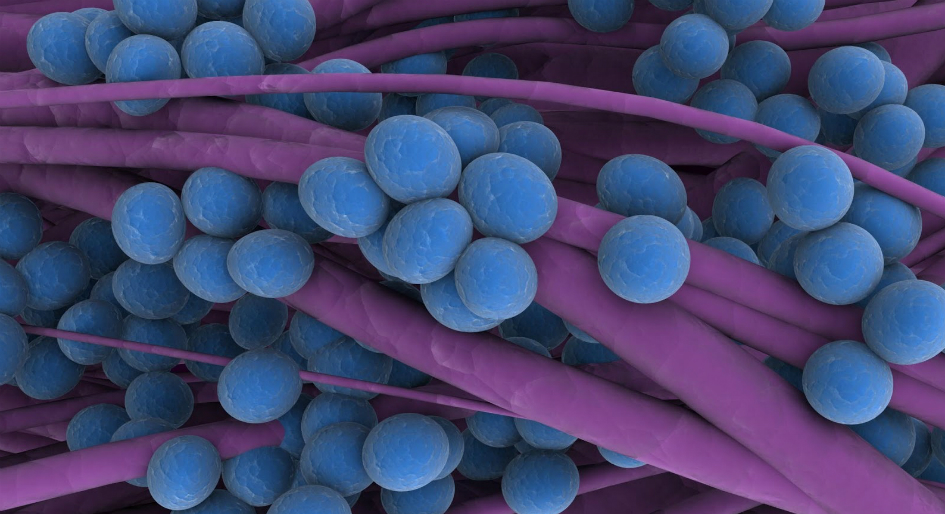
At last count, mortality due to Clostridium difficile (C-diff) infection more than tripled between 1997 and 2013, while the methicillin-resistant Staphylococcus aureus (MRSA) infection rate increased 1000 per cent from 1995 to 2009. The exact transmission route for these types of infections varies; however, a lack of proper hand hygiene and environmental contamination have both been determined to be potential sources.
Although automated UV-C disinfection has largely been targeted toward healthcare facilities, it would certainly provide similar benefits in other types of facilities where infections can be passed between occupants.
Should a facility decide to explore or implement an automated UV-C disinfection system, there are several considerations that must be taken in account. Here are four:
Consider light and shadows
UV-C disinfection uses light energy to kill microorganisms and because light is being used, shadowing becomes an important consideration. Data indicates that objects and surfaces out of direct line of sight of an UV-C emitter are less effectively disinfected. Different UV-C disinfection devices overcome this limitation in several ways. The first requires operators of the system to move the device to several locations and run multiple disinfection cycles to complete the process in each space. This methodology is simply not efficient from a labour standpoint. Other manufacturers claim that positioning a single unit in one position will reflect the UV-C energy around the room and therefore shadows are not important. This methodology is hindered by the fact that typical healthcare surfaces only reflect about 5-10 per cent of the UV-C energy, which again, makes this inefficient and results in increased disinfection cycle times. The third method to overcome shadows is to position multiple emitters in the space and allow those emitters to cover the space in a single disinfection cycle.
Consider distance
The second critical consideration is the distance of surfaces from an emitter or the overall size of the space being disinfected. As UV-C energy gets farther from an emitter, the energy drops off significantly and is therefore less effective at killing microorganisms. Again, single emitter systems are constrained by this fact and must be moved to multiple positions in the space to overcome this limitation as well. The use of multiple emitters places more surfaces in close proximity to those devices and surfaces, thereby increasing the disinfection efficiency and reducing the disinfection time required.
Consider energy amounts
A third factor to consider is whether the system delivers a calculated or measured UV-C dose or simply asks the operator to estimate the time required and set a timer. For UV-C disinfection to be effective, it must deliver enough energy to the surfaces in the room to kill the microorganism. Some microorganisms like C-diff spores are more difficult to kill and require much more energy than vegetative bacteria like MRSA. Similar to the concentration of a bleach solution, if the solution is mixed too weakly, it won’t be effective in the given contact time. Calculating or measuring the delivered dose will account for both room size and objects in the space and adjust the disinfection time accordingly.
Consider additional features
In addition to confirming whole room effective disinfection, these systems should provide additional features to make monitoring and use of the system easy. Features can include online real-time tracking and reporting systems, remote operation from outside the disinfection space, and even the ability to disinfect defined areas within different spaces to provide additional flexibility.
The World Health Organization ranked Canada as the worst developed country for hospital acquired infections in 2009, with a rate of 10.5 per cent or a 1 in 10 chance of acquiring an infection during a stay in a healthcare facility. Automated UV-C disinfection has proven to be an effective and integral component of infection prevention efforts around the world. If considering the addition of an automated disinfection system to a cleaning and infection prevention protocol, be sure to explore the different options and confirm that the system will provide effective and efficient operation for the desired goals.
Dr. Adam Buchaklian is the Director of Research and Information at Surfacide LLC, a next generation whole room automated UV-C disinfection system developer and manufacturer. Since joining Surfacide he has focused on expanding the knowledge base surrounding automated disinfection through publications and developing new tests to challenge the effectiveness of these devices. He also works with healthcare facilities to identify challenges and document the efficacy of the Surfacide UV-C disinfection system. Dr. Buchaklian can be reached at 1-844-390-3538 or Adam.Buchaklian@Surfacide.com. (www.surfacide.com)









I found it interesting when you mentioned that automated UV disinfection systems work at a genetic level. In my opinion, having new ways to reduce the lifespan and the increase of bacteria is key to our current situation. I’d be interested in learning more about how it’s done and how we can implement it in our daily lives. You did a great job explaining the benefits of UV-C disinfection systems.